Rotator Cuff Tear
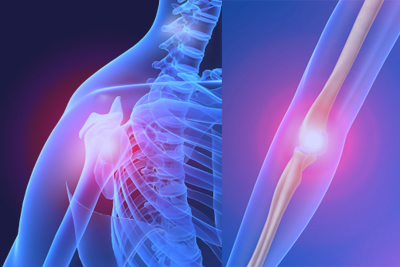
A rotator cuff tear is a common cause of pain and disability among adults. A torn rotator cuff will weaken your shoulder. This means that many daily activities, like combing your hair or getting dressed, may become painful and difficult to do.
A rotator cuff tear is a common cause of pain and disability among adults. A torn rotator cuff will weaken your shoulder. This means that many daily activities, like combing your hair or getting dressed, may become painful and difficult to do.
Your arm is kept in your shoulder socket by your rotator cuff. The rotator cuff is a network of four muscles that come together as tendons to form a covering around the head of the humerus. The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate your arm. When one or more of the rotator cuff tendons is torn, the tendon no longer fully attaches to the head of the humerus. Most tears occur in the supraspinatus muscle and tendon, but other parts of the rotator cuff may also be involved. In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
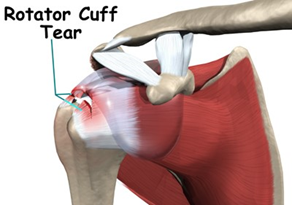
There are different types of tears.
Partial Tear. This type of tear damages the soft tissue, but does not completely sever it.
Full-Thickness Tear. This type of tear is also called a complete tear. It splits the soft tissue into two pieces. In many cases, tendons tear off where they attach to the head of the humerus, leaving a hole. There are two main causes of rotator cuff tears: injury and degeneration.
Acute Tear
If you fall down on your outstretched arm or lift something too heavy with a jerking motion, you can tear your rotator cuff. This type of tear can occur with other shoulder injuries, such as a broken collarbone or dislocated shoulder.
Degenerative Tear
Most tears are the result of a wearing down of the tendon that occurs slowly over time. This degeneration naturally occurs as we age (>40 years). Rotator cuff tears are more common in the dominant arm. If you have a degenerative tear in one shoulder, there is a greater risk for a rotator cuff tear in the opposite shoulder even if you have no pain in that shoulder. Several factors contribute to degenerative, or chronic, rotator cuff tears.
• Repetitive stress. Repeating the same shoulder motions again and again can stress your rotator cuff muscles and tendons. Baseball, tennis, rowing, and weightlifting are examples of sports activities that can put you at risk for overuse tears. Many jobs and routine chores can cause overuse tears, as well.
• Lack of blood supply. As we get older, the blood supply in our rotator cuff tendons lessens. Without a good blood supply, the body's natural ability to repair tendon damage is impaired. This can ultimately lead to a tendon tear.
• Bone spurs. As we age, bone spurs (bone overgrowth) often develop on the underside of the acromion bone. When we lift our arms, the spurs rub on the rotator cuff tendon. This condition is called shoulder impingement, and over time will weaken the tendon and make it more likely to tear.
Risk Factors
• Because most rotator cuff tears are largely caused by the normal wear and tear that goes along with aging, people over 40 are at greater risk.
• People who do repetitive lifting or overhead activities are also at risk for rotator cuff tears. Athletes especially those that play contact or overhead sports are especially vulnerable to overuse tears. Painters, carpenters, and others who do overhead work also have a greater chance for tears.
• Although overuse tears caused by sports activity or overhead work also occur in younger people, most tears in young adults are caused by a traumatic injury, like a fall.
Symptoms
The most common symptoms of a rotator cuff tear include:
• Pain at rest and at night, particularly if lying on the affected shoulder
• Pain when lifting and lowering your arm or with specific movements
• Weakness when lifting or rotating your arm
• Crepitus or crackling sensation when moving your shoulder in certain positions
Investigations
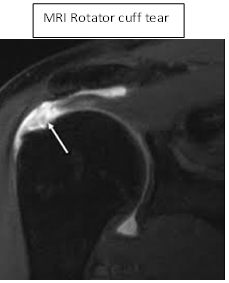
X-rays. The first imaging tests performed are usually x-rays. Because x-rays do not show the soft tissues of your shoulder like the rotator cuff, plain x-rays of a shoulder with rotator cuff pain are usually normal or may show a small bone spur.
Magnetic resonance imaging (MRI) or ultrasound. These studies can better show soft tissues like the rotator cuff tendons. They can show the rotator cuff tear, as well as where the tear is located within the tendon and the size of the tear. An MRI can also give your doctor a better idea of how "old" or "new" a tear is because it can show the quality of the rotator cuff muscles.
 Treatment
TreatmentIf you have a rotator cuff tear and you keep using it despite increasing pain, you may cause further damage. A rotator cuff tear can get larger over time. The goal of any treatment is to reduce pain and restore function. There are several treatment options for a rotator cuff tear, and the best option is different for every person. In planning your treatment, your doctor will consider your age, activity level, general health, and the type of tear you have. There is no evidence of better results from surgery performed near the time of injury versus later on. For this reason, many doctors first recommend nonsurgical management of rotator cuff tears.
Nonsurgical Treatment
In about 50% of patients, nonsurgical treatment relieves pain and improves function in the shoulder. Shoulder strength, however, does not usually improve without surgery.
Nonsurgical treatment options may include:
• Rest. Your doctor may suggest rest and limiting overhead activities. He or she may also prescribe a sling to help protect your shoulder and keep it still.
• Activity modification. Avoid activities that cause shoulder pain.
• Non-steroidal anti-inflammatory medication. Drugs like ibuprofen and naproxen reduce pain and swelling.
• Strengthening exercises and physical therapy. Specific exercises will restore movement and strengthen your shoulder. Your exercise program will include stretches to improve flexibility and range of motion. Strengthening the muscles that support your shoulder can relieve pain and prevent further injury.
• Steroid injection. If rest, medications, and physical therapy do not relieve your pain, an injection of a local anaesthetic and a cortisone preparation may be helpful. Cortisone is a very effective anti-inflammatory medicine.
Surgical Treatment
Your doctor may recommend surgery if your pain does not improve with nonsurgical methods. Continued pain is the main indication for surgery. If you are very active and use your arms for overhead work or sports, your doctor may also suggest surgery.
Other signs that surgery may be a good option for you include:
Your symptoms have lasted 6 to 12 months
You have a large tear (more than 3 cm)
You have significant weakness and loss of function in your shoulder
Your tear was caused by a recent, acute injury
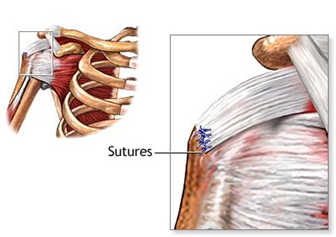
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). There are a few options for repairing rotator cuff tears. Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs. The three techniques most commonly used for rotator cuff repair include traditional open repair, arthroscopic repair, and mini-open repair. In the end, patients rate all three repair methods the same for pain relief, strength improvement, and overall satisfaction.
Open Repair
A traditional open surgical incision (several centimetres long) is often required if the tear is large or complex. The surgeon makes the incision over the shoulder and detaches the shoulder muscle (deltoid) to better see and gain access to the torn tendon. During an open repair, the surgeon typically removes bone spurs from the underside of the acromion (this procedure is called an acromioplasty). Open repair was the first technique used for torn rotator cuffs. Over the years, new technology and improved surgeon experience has led to less invasive procedures.
All-Arthroscopic Repair
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments. Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery. All-arthroscopic repair is the least invasive method to repair a torn rotator cuff. (see “Arthroscopic rotator cuff surgery” for more information)
Mini-Open Repair
The mini-open repair uses newer technology and instruments to perform a repair through a small incision. The incision is typically 3 to 5 cm long. This technique uses arthroscopy to assess and treat damage to other structures within the joint. Bone spurs, for example, are often removed arthroscopically. This avoids the need to detach the deltoid muscle. Once the arthroscopic portion of the procedure is completed, the surgeon repairs the rotator cuff through the mini-open incision. During the tendon repair, the surgeon views the shoulder structures directly, rather than through the video monitor.
Rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain shoulder strength and motion.
Immobilization
At first, the repair needs to be protected while the tendon heals. To keep your arm from moving, you will most likely use a sling and avoid using your arm for the first 4 to 6 weeks. How long you require a sling depends upon the severity of your injury.
Passive Exercise
Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises to improve range of motion in your shoulder. With passive exercise, your therapist supports your arm and moves it in different positions. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
Active Exercise
After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. Moving your muscles on your own will gradually increase your strength and improve your arm control. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program. (see “Rotator Cuff repair postoperative procotol” for more information)
Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises to improve range of motion in your shoulder. With passive exercise, your therapist supports your arm and moves it in different positions. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
Active Exercise
After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. Moving your muscles on your own will gradually increase your strength and improve your arm control. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program. (see “Rotator Cuff repair postoperative procotol” for more information)
Outcome
The majority of patients report improved shoulder strength, functional range of motion and less pain after surgery for a torn rotator cuff. Recovery can take up to 12 months. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome. Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction. Surgeon expertise is more important in achieving satisfactory results than the choice of technique.
Factors that can decrease the likelihood of a satisfactory result include:
• Poor tendon/tissue quality
• Large or massive tears
• Poor patient compliance with rehabilitation and restrictions after surgery
• Patient age (older than 65 years)
• Smoking and use of other nicotine products
• Workers' compensation claims
Complications
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anaesthesia, complications of rotator cuff surgery may include:
• Nerve injury. This typically involves the nerve that activates your shoulder muscle (deltoid).
• Infection. Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, an additional surgery or prolonged antibiotic treatment may be needed.
• Deltoid detachment. During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
• Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
• Tendon re-tear. There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Patients who re-tear their tendons usually do not have greater pain or decreased shoulder function. Repeat surgery is needed only if there is severe pain or loss of function.
The majority of patients report improved shoulder strength, functional range of motion and less pain after surgery for a torn rotator cuff. Recovery can take up to 12 months. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome. Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction. Surgeon expertise is more important in achieving satisfactory results than the choice of technique.
Factors that can decrease the likelihood of a satisfactory result include:
• Poor tendon/tissue quality
• Large or massive tears
• Poor patient compliance with rehabilitation and restrictions after surgery
• Patient age (older than 65 years)
• Smoking and use of other nicotine products
• Workers' compensation claims
Complications
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anaesthesia, complications of rotator cuff surgery may include:
• Nerve injury. This typically involves the nerve that activates your shoulder muscle (deltoid).
• Infection. Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, an additional surgery or prolonged antibiotic treatment may be needed.
• Deltoid detachment. During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
• Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
• Tendon re-tear. There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Patients who re-tear their tendons usually do not have greater pain or decreased shoulder function. Repeat surgery is needed only if there is severe pain or loss of function.


 Dr. Leonard kuo
Dr. Leonard kuo