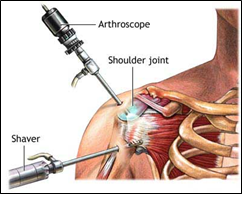
Arthroscopic shoulder surgery is used to assess and treat your shoulder condition. It is minimally invasive (key hole) surgery performed through small incisions and enables the surgeon to look into the shoulder joint, make an exact diagnosis, and in most cases treat the condition. The arthroscope is about as thick as a pencil and connects to a camera so that the surgeon can see inside the joint on a monitor. Working instruments are placed through other holes in the skin to perform the operation. Because this technique disturbs the shoulder joint less than open surgery, the hospital stay is shorter and the recovery smoother than with an open operation. On occasions, we may find something unexpected and the benefit of arthroscopy is that we can address these problems as well.
 |
Conditions that are amenable to arthroscopic treatment include: 1. Impingement of the Rotator Cuff 2. Rotator Cuff tears 3. Shoulder Instability and dislocations 4. Labral or cartilage tears 5. Chronic Frozen Shoulders 6. Early arthritis 7. Loose bodies 8. Calcific Tendonitis 9. Infections |
A week prior to surgery, you will need to cease anti-inflammatory medications and aspirin as these tablets increases your risk of postoperative bleeding. You should check with your GP to make sure that it is safe to do so. Investigations such as blood tests, ECG and chest xray may be required before the procedure.
Your admission to hospital will occur on the day of surgery. You will be seen by the Anaesthetist prior to the operation. The procedure will be done under a general anaesthetic and quite often in association with a regional nerve block. The nursing staff will also explain the use of "patient controlled analgesia" (or P.C.A.) where you regulate the amount of pain relieving medication that you use.
The operation takes about 90 minutes, depending on exactly what procedure is done. There will usually be 2 or 3 very small incisions about the shoulder. The exact operation done will depend on what is found when we look in the joint. Sometimes people have 2 or even 3 problems within the joint going on at once and all of these can usually be addressed at the same time.
You will wake up in the recovery ward with a sling and binder. The surgeon will see you the next day and explain the findings at surgery. Post operative rehabilitation will commence with the physiotherapist and this will vary depending on the exact procedure that was carried out. You will need to do those exercises at home under your own supervision about 4 times a day. You will not be required to see a physiotherapist once you leave hospital, until after I see you in the office.
It is normal to feel some discomfort with the exercises but this can be controlled with regular pain medication. The dressing will be changed and you will be permitted to shower with the operated arm by your side and go home. The sling should remain on in between exercises until I see you in the office. You should not drive until you are out of the sling.
If a postoperative appointment has not already been made, you should call the rooms to make arrangements to be reviewed 2 weeks after your operation.
You should contact the rooms earlier if you have:
• Fever above 38 degrees Celsius
• Increased pain unrelieved with pain medications
• Increased redness or swelling around the incision
• A bulge that can be felt at the shoulder
• Numbness or tingling in the arm.
• Change in motion ability
• Drainage or odour from the incision.
• Any significant concerns you have
Patients are offered the option of surgery only after non operative forms of treatment have been considered and no longer effective. It is only offered if the potential advantages of this form of treatment outweigh the possible complications and side effects. You are encouraged to consider the non-operative options of treatment and take time to make an informed choice about the preferred course of management. You are free to discuss this with me or your referring medical practitioner.
• Fever above 38 degrees Celsius
• Increased pain unrelieved with pain medications
• Increased redness or swelling around the incision
• A bulge that can be felt at the shoulder
• Numbness or tingling in the arm.
• Change in motion ability
• Drainage or odour from the incision.
• Any significant concerns you have
Patients are offered the option of surgery only after non operative forms of treatment have been considered and no longer effective. It is only offered if the potential advantages of this form of treatment outweigh the possible complications and side effects. You are encouraged to consider the non-operative options of treatment and take time to make an informed choice about the preferred course of management. You are free to discuss this with me or your referring medical practitioner.


 Dr. Leonard kuo
Dr. Leonard kuo