Slipped capital femoral epiphysis is characterised by a displacement of the capital femoral epiphysis from the femoral neck through the physeal plate. It is one of the most common disorders affecting the hip during adolescence with an incidence of 2 to 5 per 100000 and increasing as the population becomes more obese. Males are affected twice as often as females and the age range is commonly between 10 and 15 years. It affects both hips in 25-30% cases.
The femoral neck displaces anteriorly causing an apparent varus of the proximal femur. Known associations include obesity, femoral retroversion, trauma, endocrinopathy and irradiation. A positive family history is present in 5% of cases. Histologically, the physis is widened particularly in the zone of hypertrophy. The slip occurs between the zone of proliferation and zone of hypertrophy. Periosteum is stripped off the anterior neck exposing the metaphysis. Various classifications have been applied to the condition. Traditionally this was based on the duration and severity of symptoms (acute, chronic, acute on chronic). More useful is a functional classification with the hip being stable (able to bear weight) or unstable (unable to weight bear). The severity of the slip can be measured in terms of fractions or percentage of the head that has translated off the neck.
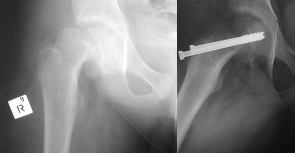
The commonest symptom is pain either in the hip, anterior thigh or knee when the diagnosis may be delayed. If the child can walk, a limp is present. The leg is often short and externally rotated with further external rotation occurring as the hip is flexed. Abduction id reduced. Radiological investigations include AP and frog lateral (not in unstable slips) xrays with characteristic features being a widened, irregular physis, trethowan’s sign, blanch sign of steel, capener’s sign and reduced neck/physeal angle. In more subtle cases, CT, bone scan or MRI may assist in the diagnosis.
Primary treatment is to stop further slippage and this is best achieved with single percutaneous cannulated screw fixation into the centre of the femoral head. The entry point needs to be anterior along the femoral neck rather than lateral. Secondary treatment aims to reduce the slip angle and improve hip mechanics. This may be achieved acutely by open reduction (surgical hip dislocation) or cuneiform osteotomy or later after physeal closure via bi-plane subtrochanteric osteotomy. This is a safer option and associated with a low incidence of avascular necrosis. Prophylactic pining is considered in pathological slips, young patients or if patients are unreliable or live in a remote location.
The prognosis is related to the degree of slip with the risk of premature osteoarthritis increasing with severity. The outcome is also suboptimal if complications such as avascular necrosis and chondrolysis develop. AVN is seen in 10-15% cases in both surgical and non-surgical cases. The incidence is increased in severe slips, if reduction is attempted (closed or open) and in acute slips.
Chondrolysis occurs in perhaps 7% cases and the cause is unknown. It is thought to have an immunological basis or be related to inadvertent pin penetration but the complication occurs also in non-surgical patients. It occurs more commonly in acute and severe slips. Symptoms include pain and stiffness with reduced joint space on x-ray. The prognosis is poor.


 Dr. Leonard kuo
Dr. Leonard kuo