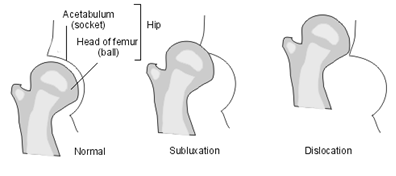
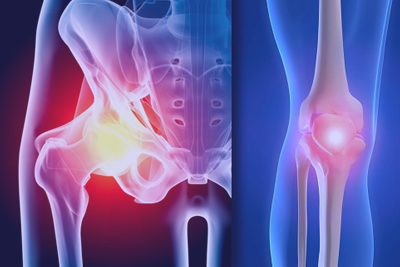
The hip joint is a ball and socket joint with a complete wrapping of soft-tissue known as the capsule. For various reasons a newborn hip may be unstable to differing degrees. Such instability of the newborn hip is known as developmental dysplasia of the hip. Where the ball of the joint (femoral head) is completely displaced from the socket (acetabulum), the term Dislocation is used. More often the femoral head is located within the acetabulum but is not completely stable. If the unstable hip is stressed, the femoral head may either dislocate completely (Dislocatable) or slip partially out of the socket (Subluxable). The dislocated, dislocatable and subluxable hips therefore represent varying degrees of instability. More infrequently a hip may be initially stable but subluxate or dislocate later because of underdevelopment of the joint (Hip dysplasia). This form of dislocation may evade early detection. Teratological Dislocation is a rare condition in which the hip has been dislocated for some months in utero before birth. It represents a difficult condition to treat.
RISK FACTORS
Infants at high risk of developmental dysplasia of the hip include those born by breech presentation, those born to families with a history of hip instability and those with deformities of feet, spine or neck. These factors are of greater significance in the female child. For instance, the risk of DDH in a female infant born by breech presentation is 1 in 35 births, while the incidence in the general population of True DDH is about 1-2 per thousand live caucasian births. DDH occurs 4-6 times more often in females.
DIAGNOSIS
The clinical examination performed by your doctor or health care sister is aimed at detecting instability as soon after birth as possible. Diagnosed early the vast majority of unstable hips can be cured by treatment. Although all children born in recognised health care institutions in this country are screened for the condition, a very small percentage of hip instability still evade detection. It is therefore advisable for infants with known risk factors to have their hips re-examined after the age of 3 months, even if the initial examination is normal. Diagnosis is made clinically and can be confirmed by special investigations such as ultrasonography and X-rays. Clinical diagnosis is difficult if the child is unsettled and more than one examination may be required. U1trasound is particularly useful in the young baby under the age of 3 months. X-rays remain an important investigation and is generally required after the age of 4 months.
GENETICS
It is quite common for newborn infants (l in 60) to show signs of hip instability immediately after birth, though the majority of hips with early instability stabilise within a week or two without treatment. Hips that remain unstable after 2 months of birth represent true developmental hip dysplasia and require treatment. DDH is the result of genetic and environmental factors. The genetic pattern is inconclusively defined but is probably of polygenetic mode. The risk to succeeding siblings of an affected child is 6 per cent where the parents are normal, and 36 per cent when one parent suffers from the condition.
TREATMENT
The goal of treatment is essentially to obtain a stable and complete (concentric) reduction of the femoral head in the acetabulum. This is consistently achieved (95%) if treatment is started within the first 6 months by positioning and maintaining the hip in a reduced position.
Brace Treatment
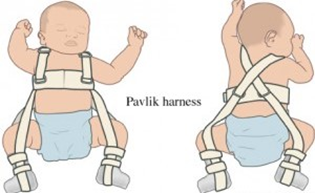
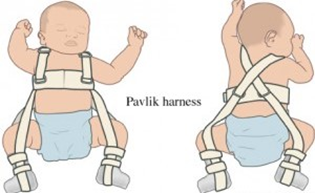
A variety of braces can be used (eg. Pavlik harness, Lorenz splint, Correctio brace) to treat the condition if diagnosis is made before the age of 6 months. Although braces differ in appearance and application, the principles of treatment are similar in all cases. All braces are designed to hold the unstable hip in a secure, reduced position. This involves positioning the hips folded up towards the abdomen (flexion) and slightly apart (abduction). The exact position varies according to the degree of instability.
Parents need to understand the management of a brace as they are inevitably involved with care of the child and brace. Attached to this article is an example of brace management (in this case a Pavlik harness). Treatment usually involves several weeks of continuous bracing until the hip is stable, after which a further period of weeks is often necessary to ensure proper development of the hip joint. The duration of treatment varies according to the age of the child when treatment is commenced and also depends on the degree of instability or dysplasia present at the start of treatment. On average most hips are braced for 3 months. Treatment although highly successful is not without complications. The most significant complication of brace treatment is a condition known as Osteonecrosis which results from loss of blood supply to a portion of the femoral head. The reported incidence of this complication varied from 0-28%. Fortunately the majority of hips affected by osteonecrosis suffer little or no long term effects. The complication can be minimised by proper adjustment of the brace to avoid excessive spreading of the thighs (abduction). The complication is more frequent where treatment is commenced late.
TREATMENT OF THE 3-12 MONTH OLD CHILD
In this age group the dislocation is usually not reducible by simple posturing of the hip in a brace. The child may be hospitalised for 1-2 weeks during which time traction is applied to the legs to stretch contracted soft-tissues that prevent reduction of the hip. Several methods of traction are available. Skin traction to suspend the legs in the air (Gallows Traction) is the most popular. The child suffers no discomfort with this treatment.
After the period of traction the child is usually brought to the operating theatre and given a short general anaesthetic to enable reduction of the hip by closed manipulation. Quite often a small operation to release the tight groin muscle (Adductor Tenotomy) is required to allow safe reduction of the hip. This operation is done through a puncture incision in the groin. Sutures are not necessary. A small amount of bleeding from the wound is usual. Most hips are successfully reduced by this treatment and X-rays with dye (arthrogram) are taken to confirm reduction of the hip.
A hip spica (see picture) is usually applied to maintain the reduction. The child remains in hospital overnight and can usually be discharged the next day. The plaster is kept on for a period of 6 weeks before the child is returned to the hospital for re-examination under an anaesthetic. Generally a second plaster is applied to be maintained for a further period of 6 weeks (Refer to addendum on Hip Spica Care). Treatment beyond this stage depends on several factors. Braces may be required for some months if development of the hip joint is inadequate.
TREATMENT OF THE OLDER CHILD WITH DDH
Treatment of DDH becomes increasingly difficult with increasing age of initial presentation. Methods for treatment vary according to age and severity of dislocation. Detailed discussion is beyond the scope of this article. Generally children at this age require operative treatment to reduce the dislocation (Open Reduction). In younger children (under the age of 2 years) soft-tissue operations are usually successful. In older children more complex operations are required including operations to the femur and pelvis eg. Femoral osteotomy, Femoral shortening, Pelvic Osteotomy etc. These are relatively major operations and some complications are known to be associated with the procedures. Success of treatment remains reasonable high but the incidence of failure and complications increases. Treatment in this age group may be prolonged.
ADDENDUM
1) MANAGEMENT OF THE PAVLIK HARNESS
This device consists of a shoulder harness and leg stirrups that have adjustable attachments (front and back straps) to the shoulder harness. It is made of canvas with velcro closures and metal buckles for attachment of the straps. It is designed to posture the hips in flexion and abduction; which is the position of reduction of the hip joint. Flexion is most important for successful reduction. Some but not excessive abduction is necessary. The chest strap should be adjusted so that it is comfortable and not so tight as to restrict breathing and feeding. The front leg straps are adjusted for flexion. At least 100 degrees of flexion is required. The back leg straps are adjusted to prevent the thighs from meeting in front and they should not be over-tightened. The transverse leg straps, the shoulder loops and the chest straps should be lifted daily to examine the underlying skin. Pressure sores are avoided by not over-tightening these straps, daily gentle massages to the underlying skin and local skin hygiene. Avoid soiling of the harness by frequent changes of nappies. Baby should not lie on the side.
DURATION OF TREATMENT
The duration of treatment varies according to the age at which treatment is commenced. Infants who receive treatment soon after birth generally require bracing for at least 6 weeks or twice their age when treatment is started. The brace is worn full time until the hip is fully stable to stress examination and this is usually after 3 weeks of treatment. Once the hip is stable, the brace is weaned off gradually. A typical regimen of weaning consists of allowing the child out of the brace for 2 hours in the first post- stable week, then adding 2 hrs each week until the child is in the brace only at night. Total period of successful bracing vary from 6 weeks to 3 months.
2) HIP SPICA CARE
The perineum should be cleaned regularly with luke warm water. Vaseline to the perineal area is helpful. Prevent soiling and wetting of the plaster. Elevate the head end of the child so that urine drains downwards. Use a hair dryer to dry the plaster that is inadvertently wetted. Change nappies more frequently than usual and do not allow wet nappies to remain on the child. Do not apply powder under-the plaster.

Infants at high risk of developmental dysplasia of the hip include those born by breech presentation, those born to families with a history of hip instability and those with deformities of feet, spine or neck. These factors are of greater significance in the female child. For instance, the risk of DDH in a female infant born by breech presentation is 1 in 35 births, while the incidence in the general population of True DDH is about 1-2 per thousand live caucasian births. DDH occurs 4-6 times more often in females.
DIAGNOSIS
The clinical examination performed by your doctor or health care sister is aimed at detecting instability as soon after birth as possible. Diagnosed early the vast majority of unstable hips can be cured by treatment. Although all children born in recognised health care institutions in this country are screened for the condition, a very small percentage of hip instability still evade detection. It is therefore advisable for infants with known risk factors to have their hips re-examined after the age of 3 months, even if the initial examination is normal. Diagnosis is made clinically and can be confirmed by special investigations such as ultrasonography and X-rays. Clinical diagnosis is difficult if the child is unsettled and more than one examination may be required. U1trasound is particularly useful in the young baby under the age of 3 months. X-rays remain an important investigation and is generally required after the age of 4 months.
GENETICS
It is quite common for newborn infants (l in 60) to show signs of hip instability immediately after birth, though the majority of hips with early instability stabilise within a week or two without treatment. Hips that remain unstable after 2 months of birth represent true developmental hip dysplasia and require treatment. DDH is the result of genetic and environmental factors. The genetic pattern is inconclusively defined but is probably of polygenetic mode. The risk to succeeding siblings of an affected child is 6 per cent where the parents are normal, and 36 per cent when one parent suffers from the condition.
TREATMENT
The goal of treatment is essentially to obtain a stable and complete (concentric) reduction of the femoral head in the acetabulum. This is consistently achieved (95%) if treatment is started within the first 6 months by positioning and maintaining the hip in a reduced position.
Brace Treatment
A variety of braces can be used (eg. Pavlik harness, Lorenz splint, Correctio brace) to treat the condition if diagnosis is made before the age of 6 months. Although braces differ in appearance and application, the principles of treatment are similar in all cases. All braces are designed to hold the unstable hip in a secure, reduced position. This involves positioning the hips folded up towards the abdomen (flexion) and slightly apart (abduction). The exact position varies according to the degree of instability.
Parents need to understand the management of a brace as they are inevitably involved with care of the child and brace. Attached to this article is an example of brace management (in this case a Pavlik harness). Treatment usually involves several weeks of continuous bracing until the hip is stable, after which a further period of weeks is often necessary to ensure proper development of the hip joint. The duration of treatment varies according to the age of the child when treatment is commenced and also depends on the degree of instability or dysplasia present at the start of treatment. On average most hips are braced for 3 months. Treatment although highly successful is not without complications. The most significant complication of brace treatment is a condition known as Osteonecrosis which results from loss of blood supply to a portion of the femoral head. The reported incidence of this complication varied from 0-28%. Fortunately the majority of hips affected by osteonecrosis suffer little or no long term effects. The complication can be minimised by proper adjustment of the brace to avoid excessive spreading of the thighs (abduction). The complication is more frequent where treatment is commenced late.
TREATMENT OF THE 3-12 MONTH OLD CHILD
In this age group the dislocation is usually not reducible by simple posturing of the hip in a brace. The child may be hospitalised for 1-2 weeks during which time traction is applied to the legs to stretch contracted soft-tissues that prevent reduction of the hip. Several methods of traction are available. Skin traction to suspend the legs in the air (Gallows Traction) is the most popular. The child suffers no discomfort with this treatment.
After the period of traction the child is usually brought to the operating theatre and given a short general anaesthetic to enable reduction of the hip by closed manipulation. Quite often a small operation to release the tight groin muscle (Adductor Tenotomy) is required to allow safe reduction of the hip. This operation is done through a puncture incision in the groin. Sutures are not necessary. A small amount of bleeding from the wound is usual. Most hips are successfully reduced by this treatment and X-rays with dye (arthrogram) are taken to confirm reduction of the hip.
A hip spica (see picture) is usually applied to maintain the reduction. The child remains in hospital overnight and can usually be discharged the next day. The plaster is kept on for a period of 6 weeks before the child is returned to the hospital for re-examination under an anaesthetic. Generally a second plaster is applied to be maintained for a further period of 6 weeks (Refer to addendum on Hip Spica Care). Treatment beyond this stage depends on several factors. Braces may be required for some months if development of the hip joint is inadequate.
TREATMENT OF THE OLDER CHILD WITH DDH
Treatment of DDH becomes increasingly difficult with increasing age of initial presentation. Methods for treatment vary according to age and severity of dislocation. Detailed discussion is beyond the scope of this article. Generally children at this age require operative treatment to reduce the dislocation (Open Reduction). In younger children (under the age of 2 years) soft-tissue operations are usually successful. In older children more complex operations are required including operations to the femur and pelvis eg. Femoral osteotomy, Femoral shortening, Pelvic Osteotomy etc. These are relatively major operations and some complications are known to be associated with the procedures. Success of treatment remains reasonable high but the incidence of failure and complications increases. Treatment in this age group may be prolonged.
ADDENDUM
1) MANAGEMENT OF THE PAVLIK HARNESS
This device consists of a shoulder harness and leg stirrups that have adjustable attachments (front and back straps) to the shoulder harness. It is made of canvas with velcro closures and metal buckles for attachment of the straps. It is designed to posture the hips in flexion and abduction; which is the position of reduction of the hip joint. Flexion is most important for successful reduction. Some but not excessive abduction is necessary. The chest strap should be adjusted so that it is comfortable and not so tight as to restrict breathing and feeding. The front leg straps are adjusted for flexion. At least 100 degrees of flexion is required. The back leg straps are adjusted to prevent the thighs from meeting in front and they should not be over-tightened. The transverse leg straps, the shoulder loops and the chest straps should be lifted daily to examine the underlying skin. Pressure sores are avoided by not over-tightening these straps, daily gentle massages to the underlying skin and local skin hygiene. Avoid soiling of the harness by frequent changes of nappies. Baby should not lie on the side.
DURATION OF TREATMENT
The duration of treatment varies according to the age at which treatment is commenced. Infants who receive treatment soon after birth generally require bracing for at least 6 weeks or twice their age when treatment is started. The brace is worn full time until the hip is fully stable to stress examination and this is usually after 3 weeks of treatment. Once the hip is stable, the brace is weaned off gradually. A typical regimen of weaning consists of allowing the child out of the brace for 2 hours in the first post- stable week, then adding 2 hrs each week until the child is in the brace only at night. Total period of successful bracing vary from 6 weeks to 3 months.
2) HIP SPICA CARE
The perineum should be cleaned regularly with luke warm water. Vaseline to the perineal area is helpful. Prevent soiling and wetting of the plaster. Elevate the head end of the child so that urine drains downwards. Use a hair dryer to dry the plaster that is inadvertently wetted. Change nappies more frequently than usual and do not allow wet nappies to remain on the child. Do not apply powder under-the plaster.



 Dr. Leonard kuo
Dr. Leonard kuo