Total Knee Replacement
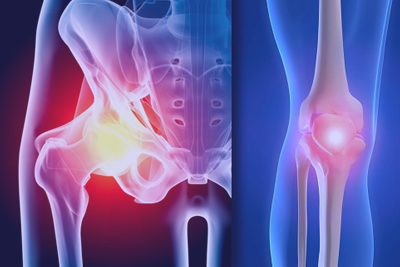
| Total knee replacement is one of the most consistently successful operation in orthopaedic surgery today. It is a procedure that is done for the severely arthritic joint when other forms of treatment no longer have any benefit. It is a ‘quality of life’ operation and performed only when a patient is significantly disabled from pain, stiffness, loss of mobility and function. It is not done for minor arthritic joint pain. The knee is a ‘hinged’ joint and bears the full weight of the body during walking. Cartilage lines the normal knee joint, allowing it to flex and extend in a smooth and free manner. In arthritis, the cartilage wears out and bone eventually grinds against bone producing pain and stiffness. When this becomes advanced, it is time to consider joint replacement. Preoperative investigations and assessment are carried out by a cardiologist physician to ensure that you are medically fit for surgery. You are admitted to hospital on the day of surgery and will be instructed in some of the simple exercises that are required after surgery: turning, coughing and deep breathing. These exercises help clear the lungs of anaesthetic and fluids that may collect. Prior to surgery, patients will receive a shave prep and an antiseptic scrub to the surgical area around the knee. The anaesthetist and surgeon will be in at some point and possibly the physiotherapist. The surgical procedure involves removing the diseased joint and replacing them with new parts. The end of the femur (thigh bone) is removed of residual cartilage and shaped to fit a metal prosthesis. The top of the tibia (leg bone) is replaced with a metal and plastic component. The patella (knee cap) may or may not be replaced. This is decided at the time of surgery. The new components are fitted together and since the painful diseased cartilage has been removed, there is generally a very quick relief of pain. The operation usually takes less than 90 minutes and the new joint is often immediately solid. During the first few days after surgery, there is naturally some pain. This can be controlled adequately by medication. Within 24 hours after surgery patients are encouraged to sit and stand. Walking is approached gradually and with supervision so as to avoid injury and complications. Emphasis is also placed on strengthening and re-educating the quadriceps muscles and improving the range of motion of the new knee. Early on, some patients may benefit from the use of a continuous passive motion machine (CPM), which flexes and extends the knee for you. Patients should continue to rehabilitate themselves for several months after the surgery to obtain the maximum benefit. As with any operation, complications may occur but fortunately this is uncommon. Blood loss requiring transfusion may be necessary after major knee surgery. This need can be reduced if anti-arthritic medications such as aspirin, anti-inflammatory medication and anticoagulant drugs are ceased at least 1 week prior to surgery. The development of deep vein thrombosis and its complications can be lessened by exercising your calf muscles regularly and with daily injections of an anticoagulant into your abdomen during the admission. Mechanical calf compressors will also be used to reduce this risk. Other complications are wound healing problems and infection. This can be minimised with the use of antibiotics around the time of surgery. Very rare problems include nerve injury, tendon rupture and fracture. By the second week, most patients feel confident enough about their mobility and ability to manage at home to be discharged. Overall, patient satisfaction with the relief of pain and return to independence is extremely high and these good results remain so for more than ten to fifteen years in over 95% of cases. 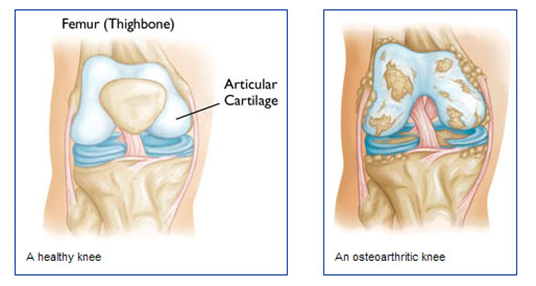 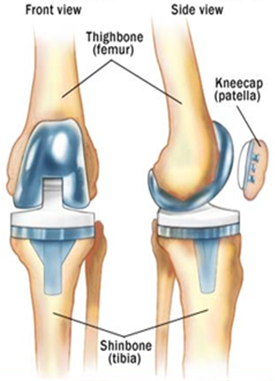 |


 Dr. Leonard kuo
Dr. Leonard kuo